How to help manage jaw clenching. What is clenched jaw? What is limited jaw opening and abnormal jaw closure? How to stop jaw clenching. How a TMJ-orofacial pain specialist can help reduce jaw clenching symptoms.
NEWS
TMJ Neck Pain: Causes, Treatment, and Prevention: Pain and tender points in the neck are common in individuals suffering from temporomandibular disorders (TMD). Treatment of jaw, neck, and orofacial pain remains a significant challenge for many healthcare providers. Clinicians must distinguish the type of pain and the probable cause of the pain to offer patients a comprehensive pain treatment plan. This article will look at how TMJ can be associated with neck pain and how to treat it.
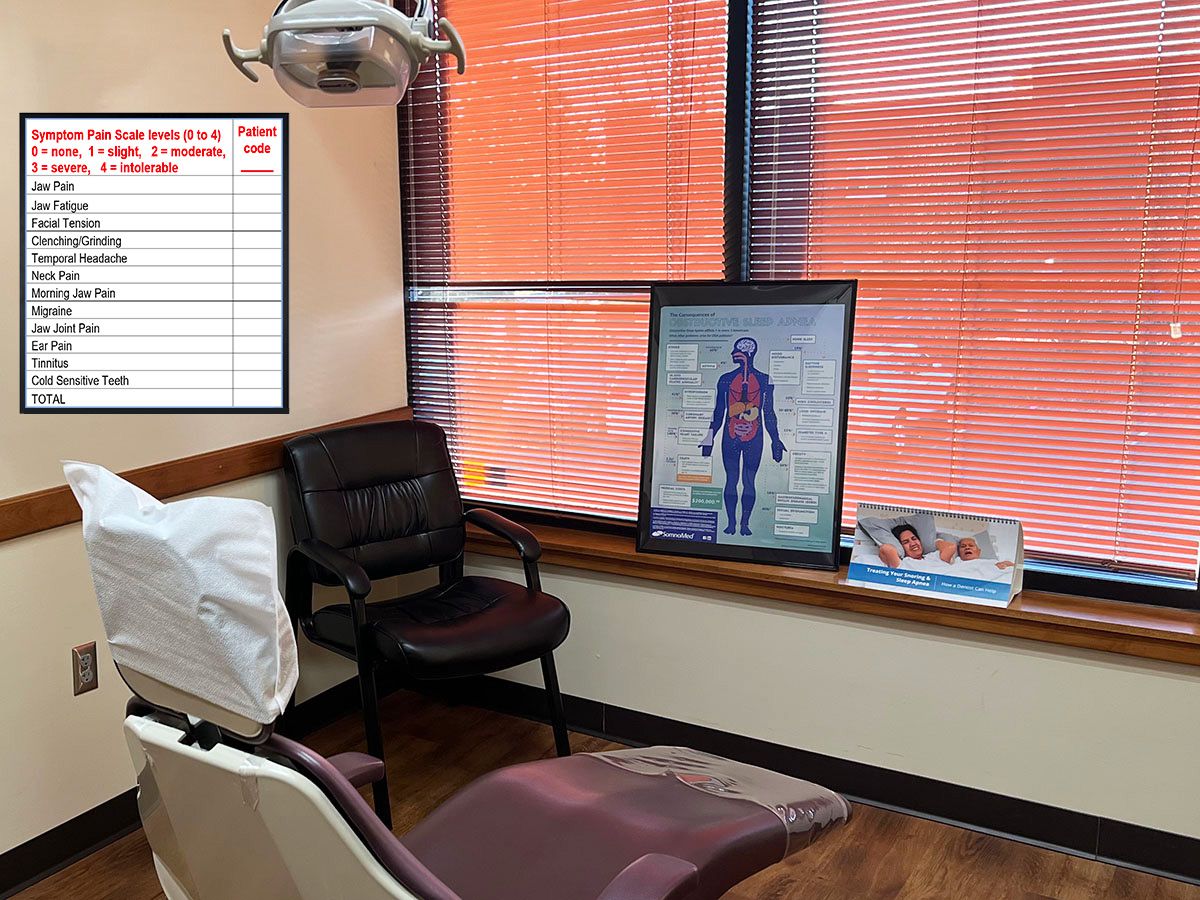
The severity of temporomandibular joint (TMJ) disorder impacts a patient’s level of pain experience and which TMJ treatment plan is recommended. The pain clinician’s skill lies in identifying the type of jaw dysfunction, probable cause, and the most conservative, effective treatment to reduce pain levels. Often, when a person is diagnosed with TMJ pain, some of the first questions are around how severe the TMJ pain may become, how quickly we can help lower their pain levels, and if this pain can be completely overcome. None of us like feeling “pain,” so we regard these as important questions to answer.
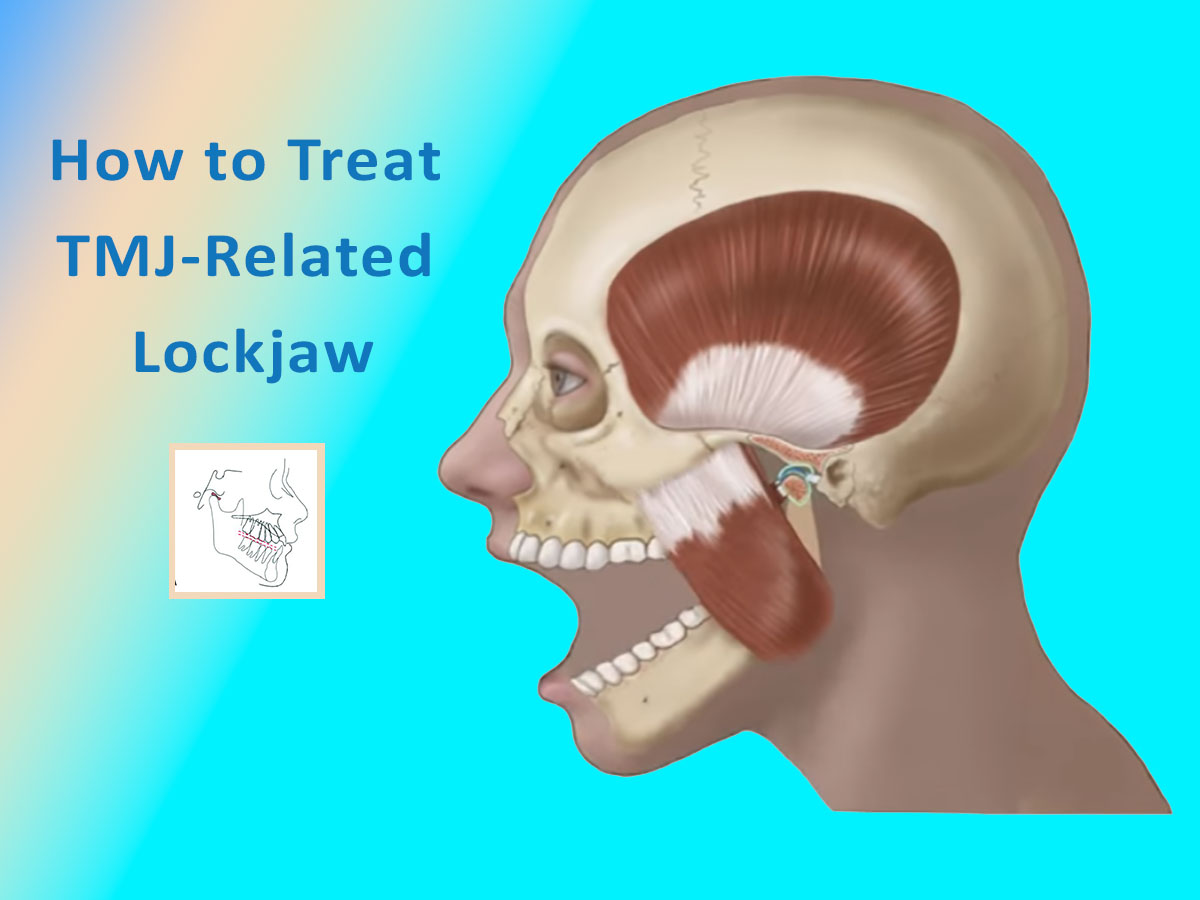
How to treat TMJ-related jaw locking up issues. Jaw locking is a common symptom of a TMJ problem, although a locked jaw sensation does not always accompany TMJ disorders or TMD. As well it can be a symptom of tetanus. This can cause confusion for people suffering from jaw pain. Patients often describe it as feeling like limited or restricted mouth opening, "jaw locking" or "jaw tension."
Non-surgical TMJ Treatments are the New Standard. The first treatment of choice for temporomandibular joint (TMJ) problems should avoid irreversible surgical treatments. Arthrocentesis occurs in three steps: forcing apart the joint constituents, washing away inflammation and degradable products, and eliminating intra-articular effusion to decrease intra-articular pressure, control pain, and improve function.
What is the Link Between TMJ Pain and Sleep Apnea? TMJ pain that impacts your ability to sleep well may lead to poor sleep quality. So, what exactly is the “link”? How does TMJ affect OSA? Sleep apnea can also lead to poor sleep quality, which can affect TMJ pain and other chronic pain conditions. Your overall health can be impacted by either TMJ or OSA; however, having both can greatly impact your daily lifestyle. Using a combination of treatments, the MN Head & Neck Pain Clinics can align the jaw to clear obstructions and strengthen jaw muscles to boost your long-term comfort.
Trigeminal Neuralgia's Association with TMJ. How is the Trigeminal Nerve Associated with TMJ? TMJ vs. TN: How to Know the Difference?
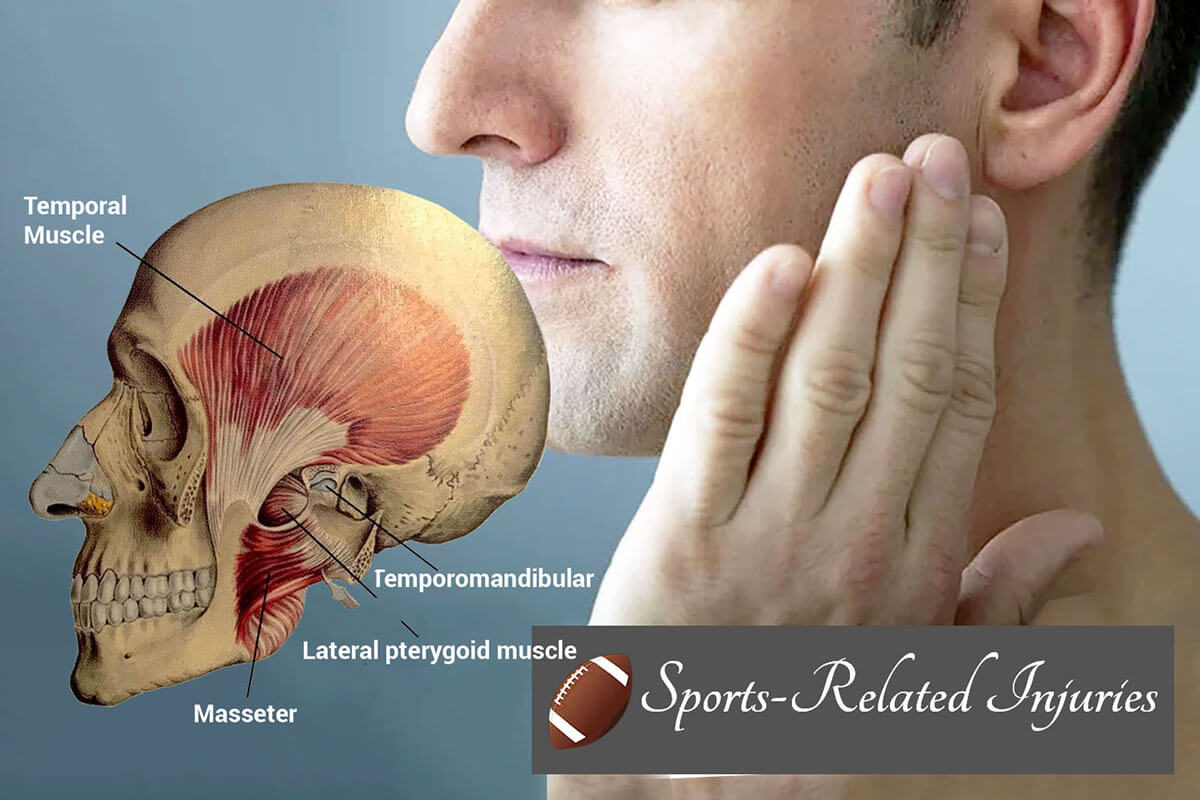
Sports-related injuries and TMJ Pain. How sports-triggered teeth clenching can lead to jaw pain. Athletes frequently have chronic pain issues. The health risks athletes face when playing contact sports. Learn about the risks of temporomandibular dysfunction among athletes. Sports-triggered teeth clenching and jaw pain
Musculoskeletal conditions are often myofascial pain related vs non-specific neck pain and can be better diagnosed. Patients with reported neck pain and tenderness upon palpation were found frequently in patients with all COPC musculoskeletal pain. Learn how our clinics can provide you with the best management of musculoskeletal conditions to reduce your neck pain.
How SSRIs can Trigger Teeth Grinding and Bruxism - Research surfaces the surprising link between using antidepressants and teeth grinding. Bruxism is a common jaw movement disorder characterized by repetitive clenching of the jaw and grinding of the teeth. Sleep bruxism is typically associated with lateral teeth grinding and significant wear on the teeth. Patients often complain of jaw pain, headaches, and tightness of the jaw when awakening, and are unaware that they are grinding and jaw clenching during their sleep. Bruxism can also occur while awake during the day.
Trigger Point Injections effectively treat the common cause of persistent pain in the jaw, neck, shoulder, back, and other areas of the body. A trigger point injection (TPI) is used as effective primary or supplemental therapy aimed at decreasing persistent pain and tightness in the musculoskeletal system. Additionally, they may be used to relieve chronic headaches associated with TMJ, migraine, and other head and neck pain conditions. But what exactly are they, and how do you know if you’d benefit from this treatment? This article will answer your questions.
Patients with Painful TMD often experience a decline in their sleep quality. A sleep evaluation is an important part of comprehensive treatment for TMD. Patients with chronic pain experience poorer sleep than healthy individuals. Sleep latency, sleep efficiency, trouble breathing during sleep, and awakenings after sleep onset can all contribute to worsening pain levels. A sustained lack of quality sleep is known to trigger higher pain levels in TMD patients.
What to Do if You Have a Pulled Jaw Muscle? A pulled jaw muscle if often an unexpected occurrence. It can trigger pain on an otherwise normal day. How do Orofacial Pain Specialists Treat Strained Jaw Muscles? When a jaw muscle is pulled or severely strained, an Orofacial Pain Specialist will establish an individualized treatment plan after diagnosing the jaw muscles and fibers in the damaged tissue. In addition to treating the pain, they will also seek to determine what caused the immediate jaw pain, inflammation, and swelling. They will treat pain resulting from trauma to the jaw.
Is Heat or Ice Better for Jaw Pain? Whether heat or cold will help you more may depend on the source of your jaw pain. TMD symptoms can be challenging to manage. If you struggle with finding jaw pain solutions, you should know the risks if left undiagnosed and treated. Many try to manage pain by using a home remedy. This may be a place to start but when more relief is needed in the long run - be quick to seek professional help. People with a temporomandibular joint disorder, or TMJ for short, are all too familiar with jaw pain. If you don't have a diagnosis yet and you’re at home or at work needing your jaw to stop hurting, you may reduce temporary jaw discomfort with the simple home remedy of applying hot or cold compresses. Let’s answer common question about if and how hot and cold packs work to provide relief from jaw pain.
How to overcome psychological distress triggered by TMJ Dysfunction. It can be challenging to remain positive during TMJ treatment when suffering from face, head, or neck chronic pain. Steps to overcome TMJ Dysfunction and related psychological distress.
Can TMJ be fixed without surgery? Yes! Non-surgical TMJ Treatment Options A non-surgical TMJ treatment approach is more conservative and is based on the unique needs of each patient.
What is TMD?
Temporomandibular joint dysfunction (sometimes abbreviated to TMD or TMJD and also termed temporomandibular joint dysfunction syndrome, temporomandibular disorder or many other names), is an umbrella term covering pain and dysfunction of the muscles of mastication (the muscles that move the jaw) and the temporomandibular joints (the joints which connect the mandible to the skull).
The most important feature is pain, followed by restricted mandibular movement, and noises from the temporomandibular joints (TMJ) during jaw movement. Although TMD is not life-threatening, it can be detrimental to the patient’s quality of life, because the symptoms can become chronic and difficult to manage. About 20% to 30% of the adult population is affected to some degree. Usually, people affected by TMD are between 20 and 40 years of age, and it is more common in females than males. TMD is the second most frequent cause of orofacial pain after dental pain (i.e. toothache). TMD is a symptom complex rather than a single condition, and it is thought to be caused by multiple factors. However, these factors are poorly understood, and there is disagreement as to their relative importance. There are many treatments available, although there is a general lack of evidence for any treatment in TMD, and no widely accepted treatment protocol exists. Common treatments that are used include the provision of occlusal splints, psychosocial interventions like cognitive behavioral therapy, and medications like analgesics (pain killers) or others. Most sources now agree that no irreversible treatment should be carried out for TMD.
Diagnosis and Management of TMD
The facial area and related cranial, oral, and dental structures are some of the most complex entities of the body. This contributes to an array of common orofacial disorders that include temporomandibular disorders (TMD), orofacial pain disorders, and orofacial sleep disorders. This site attempts to present a broad, inclusive approach to the diagnosis and management of TMD that reflects both conceptual models of human systems in understanding chronic illnesses as well as systematic reviews of treatment for successful management.
An orofacial pain specialist is the best person to diagnose and manage TMD.
Click here for a table of Common diagnoses of temporomandibular disorders (TMD) and their clinical findings.
| Some less common diagnoses of temporomandibular disorders (TMD). | |
|---|---|
| I. TMJ | |
| A. Joint pain | |
| 1. Arthritis | |
| B. Joint disorders | |
| 1. Hypomobility disorders other than disc disorders | |
| a. Adhesions/Adherence | |
| b. Ankylosis (Fibrous or Osseous) | |
| 2. TMJ dislocations | |
| C. Joint diseases | |
| 1. Systemic arthritides | |
| 2. Condylysis/Idiopathic condylar resorption | |
| 3. Osteochondritis dissecans | |
| 4. Osteonecrosis | |
| 5. Neoplasm | |
| 6. Synovial Chondromatosis | |
| D. Fractures | |
| E. Congenital/Developmental disorders | |
| 1. Aplasia | |
| 2. Hypoplasia | |
| 3. Hyperplasia | |
| II. Masticatory Muscles | |
| A. Muscle pain | |
| 1. Tendonitis | |
| 2. Myositis | |
| 3. Spasm | |
| B. Contracture | |
| C. Hypertrophy | |
| D. Neoplasm | |
| E. Movement Disorders | |
| 1. Orofacial dyskinesia | |
| 2. Oromandibular dystonia | |
| F. Masticatory muscle pain related to central/systemic pain disorder | |
| 1. Fibromyalgia/widespread pain | |
| III. Associated Structures | |
| A. Coronoid hyperplasia | |
Table puplished by NIH (Temporomandibular Disorders: Current Concepts and Controversies in Diagnosis and Management)
The National Institute of Dental and Craniofacial Research classifies TMD by the following:
-
Myofascial pain. This is the most common form of TMD. It results in discomfort or pain in the fascia (connective tissue covering the muscles) and muscles that control jaw, neck and shoulder function.
-
Internal derangement of the joint. This means a dislocated jaw or displaced disk, (cushion of cartilage between the head of the jaw bone and the skull), or injury to the condyle (the rounded end of the jaw bone that articulates with the temporal skull bone).
-
Degenerative joint disease. This includes osteoarthritis or rheumatoid arthritis in the jaw joint.
We use our jaw for so many functions, meaning that it merits attention to protect the jaw joint and prevent TMD.
Related articles:
Sleep Quality Decline in Patients with TMD
How Trigger Point Injects help Patients with Temporomandibular Joint Disorders
What is the Relationship Between Fibromyalgia and TMD?
IMAGE SOURCE: NIH: Pain profiling of patients with temporomandibular joint arthralgia and osteoarthritis diagnosed with different imaging techniques
What is the relationship between Fibromyalgia and TMD? Fibromyalgia (FM) and Temporomandibular (TMD) are two conditions that have a medical relationship to one another. It is not uncommon for a person who suffers jaw pain and headaches from TMD to also have fibromyalgia.
Increasing numbers of people with “Long-Hauler” COVID-19 now suffer from chronic pain, fatigue, and functional decline post-COVID treatment. This has increased the need for more pain management help. If you are wondering what ongoing pain conditions COVID-19 patients are facing, read this article.
Stress-induced teeth grinding increases TMJ problems; stress triggers or worsens TMDs and TMJ. COVID-19 is causing increased jaw pain cases. Stress, clenching, bruxism, and TMJ syndrome are nothing new, but they have most certainly been exacerbated by the pandemic. Find out why.
Undiagnosed TMJ Disorder causes tooth pain - symptoms, causes, and solutions. Individuals who suffer from ongoing jaw pain may develop temporomandibular.
The Dental CBCT: Why You Need More Than a Standard X-Ray Dental Cone Beam Tomography Scans and Why you Benefit from a Current X-Ray You had an x-ray at the dentist office years ago. However, you need a current dental x-ray. You still remember seeing the strange contrast of your teeth against the black background. But the last time you had a dental check-up, your dentist recommended having a cone beam CT scan (CBCT).