TEMPOROMANDIBULAR JOINT DISORDERS (TMJD)
Help for TMJ Pain
Temporomandibular joint and muscle disorders, commonly called “TMJ,” are a group of conditions that cause pain and dysfunction in the jaw joint.
This also includes the muscles that control jaw movement. We don’t know for certain how many people have TMJ disorders, but some estimates suggest that over 10 million Americans are affected. The condition appears to be more common in women than men.
For most people, pain in the area of the jaw joint or muscles does not signal a serious problem. Generally, discomfort from these conditions is occasional and temporary, often occurring in cycles. The pain eventually goes away with little or no treatment. Some people, however, develop significant, long-term symptoms. An orofacial therapeutics specialist can help diagnose and treat. However, you can proactively protect yourself by understanding common symptoms of a pulled jaw muscle.
When you Need TMJ Pain Solutions
If you have questions about TMJ disorders, you are not alone. Researchers, too, are looking for answers to what causes these conditions and what the best treatments are. Until we have scientific evidence for safe and effective treatments, it’s important to avoid, when possible, procedures that can cause permanent changes in your bite or jaw.
What is the Temporomandibular joint?
The temporomandibular joint connects the lower jaw, called the mandible, to the bone at the side of the head—the temporal bone. If you place your fingers just in front of your ears and open your mouth, you can feel the joints. Because these joints are flexible, the jaw can move smoothly up and down and side to side, enabling us to talk, chew and yawn. Muscles attached to and surrounding the jaw joint control its position and movement.
When we open our mouths, the rounded ends of the lower jaw, called condyles, glide along the joint socket of the temporal bone. The condyles slide back to their original position when we close our mouths. To keep this motion smooth, a soft disc lies between the condyle and the temporal bone. This disc absorbs shocks to the jaw joint from chewing and other movements. Tooth pain may indicate a hidden TMD issue.
The temporomandibular joint is different from the body’s other joints. The combination of hinge and sliding motions makes this joint among the most complicated in the body. Also, the tissues that make up the temporomandibular joint differ from other load-bearing joints, like the knee or hip. Because of its complex movement and unique makeup, the jaw joint and its controlling muscles can pose a tremendous challenge to both patients and health care providers when problems arise.
What are TMJ disorders?
Disorders of the jaw joint and chewing muscles—and how people respond to them—vary widely. Researchers generally agree that the conditions fall into three main categories:
- Myofascial pain involves discomfort or pain in the muscles that control jaw function.
- Internal derangement of the joint involves a displaced disc, dislocated jaw, or injury to the condyle.
- Arthritis refers to a group of degenerative/inflammatory joint disorders that can affect the temporomandibular joint.
A person may have one or more of these conditions at the same time. Some people have other health problems that co-exist with TMJ disorders, such as chronic fatigue syndrome, sleep disturbances, or fibromyalgia, a painful condition that affects muscles and other soft tissues throughout the body. A clear, established link between TMJ and sleep apnea exists, as well as an association between TMD and fibromyalgia. These disorders share some common symptoms, which suggests that they may share similar underlying mechanisms of disease. However, it is not known whether they have a common cause.
Rheumatic disease, such as arthritis, may also affect the temporomandibular joint as a secondary condition. Rheumatic diseases refer to a large group of disorders that cause pain, inflammation, and stiffness in the joints, muscles, and bone. Arthritis and some TMJ disorders involve inflammation of the tissues that line the joints. The exact relationship between these conditions is not known.
How jaw joint and muscle disorders progress is not clear. What this video to view normal TMJ in motion. Your jaw joint should function in this manner – with all jaw muscles, tendons, and ligaments doing their job without stress.
Symptoms worsen and ease over time, but what causes these changes is not known. Most people have relatively mild forms of the disorder. Their symptoms improve significantly, or disappear spontaneously, within weeks or months. For others, the condition causes long-term, persistent and debilitating pain.
What are Signs and Symptoms of TMJ Disorders?
A variety of symptoms may be linked to TMJ disorders. Pain, particularly in the chewing muscles and/or jaw joint, is the most common symptom. Other likely symptoms include:
- radiating pain in the face, jaw, or neck,
- jaw muscle stiffness,
- limited movement or locking of the jaw,
- painful clicking, popping or grating in the jaw joint when opening or closing the mouth,
- a change in the way the upper and lower teeth fit together.
“It has been shown in the scientific literature that the most common signs and symptoms of TMD patients are pain and the articular limitation of jaw motion; these might even induce disability during activities of daily living (e.g., talking, swallowing, etc.) with a consequent reduction in health-related quality of life.” – NIH: Temporomandibular Disorders: Current and Future Concepts in Diagnosis and Management, January 2023
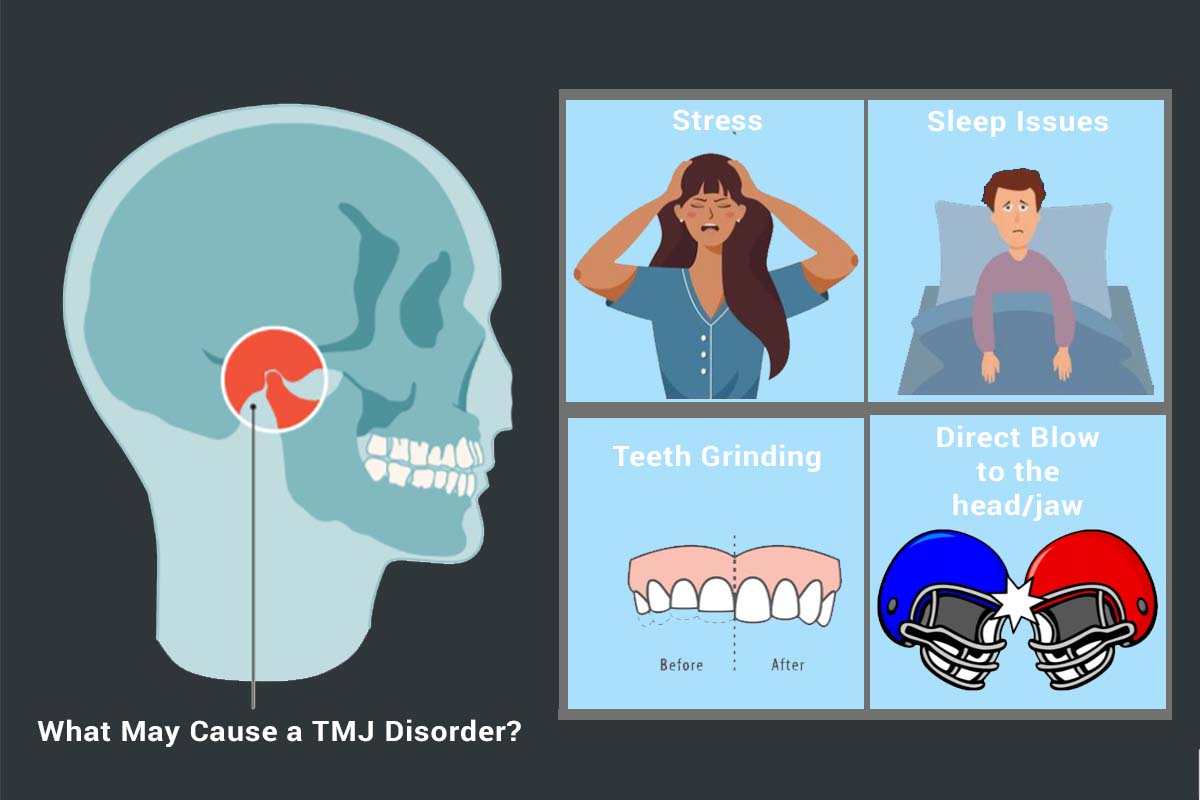
What Causes TMJ Disorders?
Trauma to the jaw or temporomandibular joint plays a role in some TMJ disorders. But for most jaw joint and muscle problems, scientists don’t know the causes. Because the condition is more common in women than in men, scientists are exploring a possible link between female hormones and TMJ disorders.
For many people, symptoms seem to start without obvious reason. Research disputes the popular belief that a bad bite or orthodontic braces can trigger TMJ disorders. If left untreated, psychological distress brought on by TMJ Dysfunction can set in and add to a patient’s stress.
There is no scientific proof that sounds—such as clicking—in the jaw joint lead to serious problems. In fact, jaw sounds are common in the general population. Jaw noises alone, without pain or limited jaw movement, do not indicate a TMJ disorder and do not warrant treatment. However, if your trigeminal nerve is affected, it is a matter of concern. Where your face is affected by pain will tell your orofacial pain specialist if the trigeminal nerve is involved.
The etiology of TMD is multifactorial; risk factors can include:
- Excessive muscle tension
- Teeth grinding.
- Teeth clenching as a parafunctional activity.
- Repetitive trauma to the jaw joint.
- Bruxism.
- Psychological and emotional distress may add to TMJ pain.
- Anxiety and depression might lead to the development and/or exacerbation of pain.
How are TMJ disorders diagnosed?
There is no widely accepted, standard test now available to correctly diagnose TMJ disorders. Because the exact causes and symptoms are not clear, identifying these disorders can be difficult and confusing. Currently, health care providers note the patient’s description of symptoms, take a detailed medical and dental history, and examine problem areas, including the head, neck, face, and jaw. Imaging studies may also be recommended.
You may want to consult your doctor to rule out other known causes of pain. Facial pain can be a symptom of many conditions, such as sinus or ear infections, various types of headaches, and facial neuralgias (nerve-related facial pain). Ruling out these problems first helps in identifying TMJ disorders.
The diagnosis is often conducted according to DC/TMD and through cone beam computer tomography, magnetic resonance imaging exams, and physical examination by a TMJ expert. Depending on the extent of pain, perceived injury, and possible secondary medical conditions, the diagnosis process of temporomandibular joint (TMJ) disorders is determined case by case.
How are TMJ disorders treated?
Because more studies are needed on the safety and effectiveness of most treatments for jaw joint and muscle disorders, experts strongly recommend using the most conservative, reversible treatments possible. Conservative treatments do not invade the tissues of the face, jaw, or joint, or involve surgery. Reversible treatments do not cause permanent changes in the structure or position of the jaw or teeth. Even when TMJ disorders have become persistent, most patients still do not need aggressive types of treatment.
You may find myofascial release treatment for TMJ pain helpful. Many do.
Conservative Treatments
Because the most common jaw joint and muscle problems are temporary and do not get worse, simple TMJ treatment may be all that is necessary to relieve discomfort.
Self-Care Practices
There are steps you can take that may be helpful in easing symptoms, such as:
- eating soft foods,
- applying ice packs,
- avoiding extreme jaw movements (such as wide yawning, loud singing, and gum chewing),
- learning techniques for relaxing and reducing stress,
- practicing gentle jaw stretching and relaxing exercises that may help increase jaw movement. Your health care provider or a physical therapist can recommend exercises if appropriate for your particular condition.
Pain Medications
For many people with TMJ disorders, short-term use of over-the-counter pain medicines or nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may provide temporary relief from jaw discomfort. When necessary, your dentist or physician can prescribe stronger pain or anti-inflammatory medications, muscle relaxants, or anti-depressants to help ease symptoms.
Stabilization Splints
Your physician or dentist may recommend an oral appliance, also called a stabilization splint or bite guard, which is a plastic guard that fits over the upper or lower teeth. Stabilization splints are the most widely used treatments for TMJ disorders. Studies of their effectiveness in providing pain relief, however, have been inconclusive. If a stabilization splint is recommended, it should be used only for a short time and should not cause permanent changes in the bite. If a splint causes or increases pain, symptoms of cluster headaches, or affects your bite, stop using it and see your health care provider.
The conservative, reversible treatments described are useful for temporary relief of pain – they are not cures for TMJ disorders. If symptoms continue over time, come back often, or worsen, tell your doctor. Evidence shows that mouth guards can help encourage the jaw to relax during the night (especially for the individual whose TMJ pain is worse in the morning).
TMJ injuries during contact sports also often benefit from the stabilization of a TMJ splint.
Botox
Botox® (botulinum toxin type A) is a drug made from the same bacterium that causes food poisoning. Used in small doses, Botox injections can actually help alleviate some health problems and have been approved by the Food and Drug Administration (FDA) for certain disorders. However, Botox is currently not approved by the FDA for use in TMJ disorders. Oral appliances are a more proven short-term treatment method.
Results from recent clinical studies are inconclusive regarding the effectiveness of Botox for the treatment of chronic TMJ disorders. Additional research is underway to learn how Botox specifically affects jaw muscles and their nerves. The findings will help determine if this drug may be useful in treating TMJ disorders or other pain disorders.
Irreversible Treatments
Irreversible treatments that have not been proven to be effective – and may make the problem worse – include orthodontics to change the bite; crown and bridgework to balance the bite; grinding down teeth to bring the bite into balance, called “occlusal adjustment”; and repositioning splints, also called orthotics, which permanently alter the bite.
We do know that stress-triggered grinding of the teeth increases the likelihood TMJ problems.
Surgery to resolve TMJ pain
Other types of treatments, such as surgical procedures, invade the tissues. Surgical treatments are controversial, often irreversible, and should be avoided where possible. There have been no long-term clinical trials to study the safety and effectiveness of surgical treatments for TMJ disorders. Nor are there standards to identify people who would most likely benefit from surgery.
Failure to respond to conservative treatments, for example, does not automatically mean that surgery is necessary. If surgery is recommended, be sure to have the doctor explain to you, in words you can understand, the reason for the treatment, the risks involved, and other types of treatment that may be available.
Jaw Joint Implants
Surgical replacement of jaw joints with artificial implants may cause severe pain and permanent jaw damage. Some of these devices may fail to function properly or may break apart in the jaw over time. If you have already had temporomandibular joint surgery, be very cautious about considering additional operations. Persons undergoing multiple surgeries on the jaw joint generally have a poor outlook for normal, pain-free joint function. Before undergoing any surgery on the jaw joint, it is extremely important to get other independent opinions and to fully understand the risks.
MN Head & Neck Clinic to Gain TMJ disorder help: 763-577-2484
Additional Recommended Reading
The U.S. Food and Drug Administration (FDA) monitors the safety and effectiveness of medical devices implanted in the body, including artificial jaw joint implants. Patients and their health care providers can report serious problems with TMJ implants to the FDA through MedWatch at www.fda.gov/medwatch or telephone toll-free at 1-800-332-1088. Consider ways to treat your jaw without surgery.
DISORDERS WE TREAT
OROFACIAL PAIN
The specialty of Orofacial Pain is concerned with the prevention, evaluation, diagnosis, treatment, and rehabilitation.
READ MORE ›
HEADACHES
There are four types of headache: vascular, muscle contraction (tension), traction, and inflammatory.
READ MORE ›
FACIAL NERVE PAIN
Trigeminal neuralgia is a chronic pain condition that causes extreme, sporadic, sudden burning or shock-like face pain.
READ MORE ›
TMJD
TMJ is a group of conditions that cause pain and dysfunction in the jaw joint and the muscles that control jaw movement.
READ MORE ›
ORAL APPLIANCE THERAPY
Sleep apnea is the most common sleep disorder, affecting nearly 1 out of every 8 individuals.
READ MORE ›
NECK PAIN
Neck muscles can be strained from poor posture — whether it’s leaning over your computer or hunching over your workbench.
READ MORE ›