TMJ Pain Severity
Effects of TMJ Pain Severity
The severity of temporomandibular joint (TMJ) disorder impacts a patient’s level of pain experience and which TMJ treatment plan is recommended.
The pain clinician’s skill lies in identifying the type of jaw dysfunction, probable cause, and the most conservative, effective treatment to reduce pain levels.
Often, when a person is diagnosed with TMJ pain, some of the first questions are around how severe the TMJ pain may become, how quickly we can help lower their pain levels, and if this pain can be completely overcome. None of us like feeling “pain,” so we regard these as important questions to answer.
Table of Contents
- Effects of TMJ Pain Severity
- How are craniofacial pain and myofascial pain different?
- Can TMJ cause severe facial pain?
- What is Myofascial Pain Dysfunction Syndrome of TMJ?
- Pharmacological Management For Chronic Myofascial Pain
- SUMMARY: Seek Help Before Your TMJ Pain Becomes Severe
How are craniofacial pain and myofascial pain different?
Craniofacial pain and myofascial pain may share trigger points that cause pain when pressure is applied. However, they are different medical conditions.
Craniofacial pain commonly varies from mild to severe headaches, facial pain, neck and upper back tension, dizziness, and jaw-locking pain.
Myofascial pain differs in that it is a painful condition that originates from muscle and surrounding fascia tissue. It commonly causes localized jaw pain in a restricted area or referred fascial pain.
We understand why understanding myofascial, craniofacial, and fibromyalgia pain may feel similar. It is important to distinguish the different causes in order to come up with the right treatment. Fibromyalgia pain often occurs throughout your entire body, whereas myofascial pain occurs in one specific area.
For example, if the pain comes from an overextended time having your mouth open at the dentist, that can be a cause of the jaw pain. Scholarly studies suggest that after evaluating temporomandibular joint disorder in partially versus completely edentulous patients found a correlation between those with TMD symptoms following tooth loss. Both the intensity and frequency of pain increased in proportion to the number of teeth removed. [1]
Can TMJ cause severe facial pain?
Because people’s nerves and muscles are so complex in the head, neck, and jaw area, when these muscles spasm, problems can be extensive. Because pain in this area can be referred to as pain, people who suffer from TMJ pain symptoms benefit from an orofacial pain specialist’s help to best determine the cause of their severe facial pain.
Even your neck, shoulder, and upper back muscles can become involved when left untreated. Minor TMJ discomfort may go away without treatment; however, severe facial pain needs immediate medical care. Injury to your jaw or temporomandibular joint can lead to TMDs more severe pain. Chronic TMD, especially myofascial TMD, is considered a functional pain syndrome.
TMJ can erode the joint capsule between the skull and jawbone, causing increased pain severity. TMDs are primarily characterized by pain.
“For some patients, the pain in the TMJ is severe and unrelenting.” – fda.gov, Temporomandibular Disorders (TMD) Devices [2]
What is Myofascial Pain Dysfunction Syndrome of TMJ?
Temporomandibular Myofascial Pain Syndrome is typically triggered by muscle tension, fatigue, or (less often) spasms in the masticatory muscles. Symptoms may include severe, constant, and dull facial muscle pain. Patients often report constant pain in the affected area.
TMJPDS is a pain disorder characterized by spontaneous pain and jaw function-induced pain in the joint and muscles of mastication of the TMJ. Because of the interplay between the muscles and joints, a problem with either one can lead to stiffness, headaches, ear pain, malocclusion, clicking sounds, or trismus. [3]
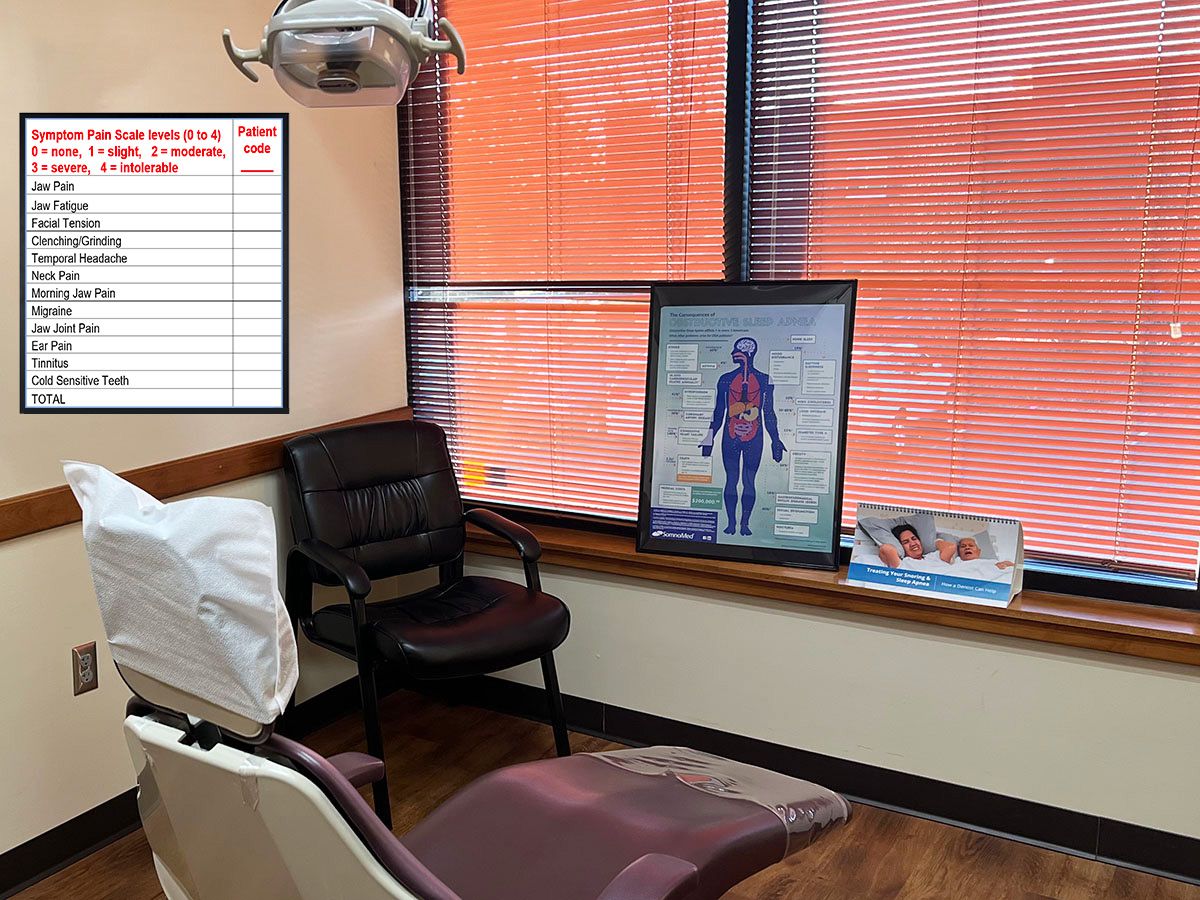
The National Institute of Dental and Craniofacial Research provides the following table explaining “Simple” to “Complex” TMD treatment based on a patient’s pain severity.
| Table of Simple” to “Complex” TMD Treatment Options Based on Patient Pain Severity Level | |||
|---|---|---|---|
| SIMPLE | COMPLEX | ||
| Simplest Treatments; try these treatments first | Could be prescribed by a practitioner or dentist as a second step in simple treatments do not help | Proceed with caution if these treatments are recommended | Only consider these if the doctor or dentist recommends them as a last resort; ask for a second opinion. Involved direct access and permanent changes to the jaw joint |
| Eating soft foods
Applying heat or cold to jaw or face Jaw stretching or strengthening exercises Short-term, over-the-counter NSAIDS Self-management |
Behavioral health approaches
Physical therapy, including manual therapy Prescription medications Complementarytreatments |
Prolotherapy injections
Arthrocentesis (also called joint aspiration) Arthroscopy (procedure for diagnosing and treating joint problems) |
Surgery, including TMJ implants |
Can TMJ affect cranial nerves?
Severe TMJ pain can directly or indirectly impact your cranial nerves. Your trigeminal nerve is the fifth cranial nerve (CN V) you have. It is also the largest of your cranial nerves. TMJ pain is transmitted mainly through this nerve and can result in other pain throughout the head and neck. Some of the symptoms of TMJ issues can be directly attributed to strained interaction with your trigeminal nerve.
Signs of internal derangement of the TMJ include clicking noises and lateral displacement of the “meniscus.” Your meniscus is a tiny piece of disc-shaped cartilage. It functions as a needed cushion between the mandibular condyle and the glenoid fossa in TMD. Your meniscus is the part of your TMJ that your jaw relies on to open wide, move up and down, forward and back, and for normal side-to-side jaw movements.
Internal derangements may occur if this disk is altered and the diskal ligaments become elongated. The severity of the derangement depends on the extent of the disk and ligament changes. If the disk placement remains anterior to the condyle, the derangement is said to be without reduction. [4]
What is the difference between TMD and TMJ pain severity?
Temporomandibular disorders (TMDs) consist of a group of more than 30 conditions that cause pain and dysfunction in the jaw joint and muscles that control jaw movement. “TMDs” refers to the disorders, and “TMJ” refers only to the temporomandibular joint itself. You have two TMJs, one on each side of your jaw. Severe TMJ pain more commonly indicates a TMD condition.
What are the neurological symptoms of TMJ?
If we look beyond the common temporomandibular joint dysfunction symptom, neurological symptoms may be more challenging to diagnose.
TMJ-related neurological pain symptoms may include:
- Chronic headaches – severe headaches in the temple region or behind your eyes may signal a TMJ issue. These headaches can feel like severe debilitating pain and traditional headache treatments sometimes fail.
- Recurring dizziness – TMJ patients that experience lightheadedness or dizziness, notably when moving the head or standing up.
- Facial pain – TMJ discomfort may extend to pain and discomfort in the face, especially in a person’s jaw, cheekbones, and temples.
- Persistent tingling or numbness – more severe TMJ pain may be accompanied by tingling or numbness in the face or jaw.
- Persistent neck pain – Unrelenting pain and stiffness in the neck and shoulder area can be a sign of TMJ.
- Cognitive reasoning challenges – When TMJ pain becomes moderate to severe, it has been linked to cognitive issues such as memory loss, difficulty concentrating, and a feeling of brain fog. [5]
Pharmacological Management For Chronic Myofascial Pain
Chronic refractory myofascial pain (CRMP) is a neuro musculoskeletal condition needing integrated and innovative pain management. Chronic myofascial pain syndrome (MPS) typically has a more challenging prognosis, and the symptoms can last for six months or longer.
Non-opiate analgesics and non-steroidal anti-inflammatory drugs (NSAIDs) or SSRIS may be medically necessary for moderate to severe inflammatory conditions and pain. When necessary for the treatment of chronic pain, sleep disturbance, and nocturnal bruxism, optimal pain relief at prescribed doses is carefully managed.
After a diagnosis, we may first recommend trigger point injections, myofascial release, and/or muscle relaxants. Our pain specialists start with a conservative approach and offer recommendations that are considered medically necessary in refractory pain.
Severity of TMJ pain and dysfunction
Your TMJ pain severity levels and causation, among other factors, help determine your recommended treatment.
The Wilkes staging system for TMJ ID provides a guide for treatment based on the pain severity and the joint damage. TMJ ID is defined in the following four stages:
Table: Guide for TMJ Treatment Based on Pain Severity |
||
|---|---|---|
| Stage | Clinical findings | Radiological findings |
| I (Early) | Painless clicking, no limitation of motion | Slight disc displacement with early reduction, normal disc morphology |
| II (Early/intermediate) | Occasional painful clicking, intermittent locking, related headache | Moderate disc displacement with late reduction, mild disc deformity |
| III (Intermediate) | Frequent pain, joint tenderness, restriction of motion, closed locks | Disc displacement without reduction, deformity of disc, no hard tissue changes |
| IV (Intermediate/late) | Chronic pain, restriction of motion | Severe disc displacement (without reduction), Severe deformity of disc, degenerative changes |
| V (Late) | Variable and episodic joint pain, chronic restriction of motion, crepitus | Gross deformity and/or perforation of disc, degenerative arthritic changes, osteophyte deformity subcortical cyst formation |
Does TMJ get progressively worse?
Yes, without an early diagnosis and treatment plan, TMJ conditions can cause progressive and continuous changes in the occlusion and jaw relationships.
Another example is someone struggling with bruxism, which can cause facial pain and discomfort in the jaw and temporomandibular joint. On-going and excessive pressure on these areas can contribute to a TMJ disorder developing or worsening. A person’s harmful patterns of teeth grinding, psychological stress, or an untended injury to the jaw can lead to further pain and progressively more limitations in jaw movement.
Can life-stresses make TMJ pain more severe?
Yes, stress and anxiety can escalate TMJ pain. Experiencing night after night of restless, stress-induced sleep can mean you are grinding your teeth and jaw clenching unconsciously. This, in turn, causes muscle tension in the jaw area. It’s vital to monitor muscle activation if opioids or other medications are prescribed to help manage stress-triggered pain, anxiety, and depression.
Some medications like SSRIs can aggravate sleep bruxism.
Avoid the dangers of untreated TMJ
The point is – don’t wait until your jaw or facial pain escalates.
SUMMARY: Seek Help Before Your TMJ Pain Becomes Severe
While Temporomandibular joint pain dysfunction syndrome has diverse clinical presentation and can be distressing, it responds to early and effective conservative pain management.
If you or someone in your care suffers from TMJ, jaw locking, head, neck, or myofascial pain, the Minnesota Head and Neck Pain Clinics are here to help.
Call the MN Head & Neck Clinic to gain help today: (763) 577-2484
Resources
[1] M. Moaleem, April 2017, “Prevalence and Severity of Temporomandibular Joint Disorders”, https://www.semanticscholar.org/paper/Prevalence-and-Severity-of-Temporomandibular-Joint-Moaleem-Aldhalai/63b7df711d2b96987962c6aa7ed0b872c6e9f52f
[2] OM Eweka, et al., “Temporomandibular Pain Dysfunction Syndrome in Patients Attending Lagos University ,” March 2026, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5342624/
[3] FDA staff, “Temporomandibular Disorders (TMD) Devices,” current, https://www.fda.gov/medical-devices/dental-devices/temporomandibular-disorders-tmd-devices
[4] Gary Klassar, “Internal Temporomandibular Joint (TMJ) Derangement,” Sept 2023, https://www.merckmanuals.com/professional/dental-disorders/temporomandibular-disorders/internal-temporomandibular-joint-tmj-derangement
[5] Michael Pruett, “The Impact Of TMJ On Neurological Function,” March 2023, https://johnagarzadds.com/tmj-neurological-symptoms/


