Myofascial Release for TMJ Pain
Myofascial Release for TMJ Pain
Whether your pain is triggered by TMD or chronic myofascial pain, you can benefit from professional orofacial pain management.
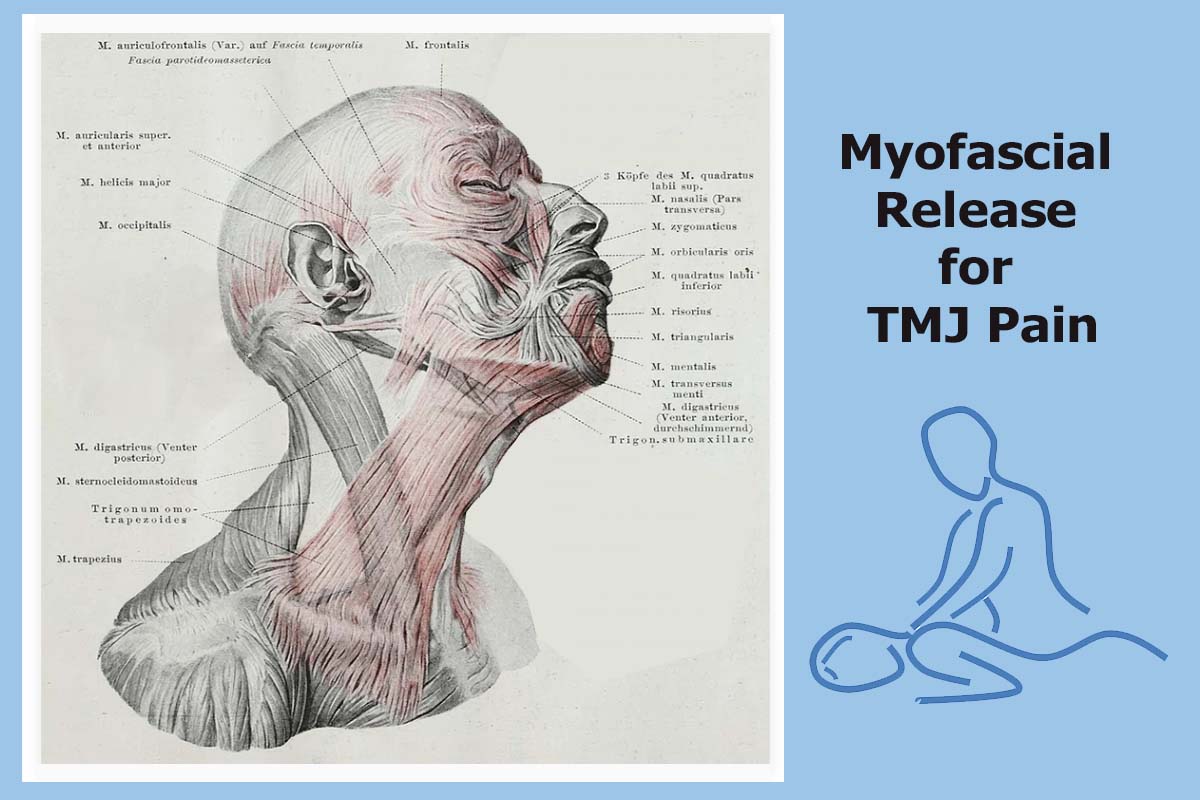
Your fascial area is made up of solid (muscles) and liquid (blood, lymph) elements and components that comprise contractile muscle tissue and connective tissue. The myofascial system contains the nervous, vascular tissue, and the lymphatic system, which is why it can influence your overall well-being. This helps explain why myofascial release can be so beneficial.
Table of Contents
- What is Myofascial Release for Jaw Pain?
- Is TMJ the Same as Myofascial Pain?
- Is Myofascial Pain a Chronic Pain Disorder?
- Do I need a prescription to manage chronic myofascial pain?
- What are intraoral myofascial therapies?
- Does myofascial massage increase blood flow?
- Does limited jaw opening indicate a jaw neuromuscular issue?
- Can someone with jaw pain do self-myofascial release exercises?
- Is myofascial release better than deep tissue massage?
- Myofascial Release Techniques Aimed to Improve ROM
- CONCLUSION: When to see a Pain Specialist for TMJ Pain?
What is Myofascial Release for Jaw Pain?
Myofascial release (MFR) generally addresses specific areas in the fascia.
It helps tense muscles around the jaw relax through massage techniques. This type of physical therapy massage technique typically alleviates pain within the affected muscles. Many patients with temporomandibular joint disorder (TMD) find that this decreases pain and inflammation, as well as improves the mobility of the jaw.
Myofascial Release treatment intended for the TMJ structure encompasses gentle manipulation of the cranial and jaw tissues to release muscle tension. We also know that self-reported awake bruxism (AB) has been associated with temporomandibular disorders (TMD). For example, during a Bruxism Risk Assessment, specific palpation of connecting facial bones that act as levers will also release jaw tension.
Proper myofascial palpation with a symmetrical balance can even create a general feeling of well-being. This is because our marvelously created human brains move in a physiological cycle. Myofascial release (MFR, self-myofascial release) is widely used for treating skeletal muscle immobility and pain by relaxing contracted muscles, improving blood and lymphatic circulation, and building your muscles’ stretch reflex.
Is TMJ the Same as Myofascial Pain?
Chronic myofascial pain may surface in people with TMD or in individuals whose temporomandibular joint (TMJ) functions normally. TMJ can create mild symptoms of discomfort, while it can be painful for others. Jaw muscle tension, fatigue, or misalignment – and even spasms can cause it. It is more common in women, and it is a chronic disorder.
Myofascial pain syndrome is more commonly the source of temporomandibular pain than TMJ derangement. Tension, fatigue, and even spasming of the masticatory muscles may result from parafunctional behavior (meaning bruxism) or a sports-related injury to the jaw. It is a disease with currently no widely accepted standard management and surveillance protocol.
The National Institute of Dental and Craniofacial Research (NIDCR) classifies TMD by the presence of myofascial pain. This is the most common form of TMD. It results in discomfort or pain in the connective tissue covering the muscles (fascia) and the muscles that control jaw, neck, and shoulder function. [1]
Is Myofascial Pain a Chronic Pain Disorder?
Yes. Myofascial pain syndrome comprises both acute and chronic pain. [2] The pain can be intense in addition to deep and aching. While it’s focused on a muscle, it may also radiate to other parts of the body. People suffering from this disorder often have a tender knot in a specific muscle accompanied by pain that worsens over time. Commonly, people begin experiencing sleep difficulties because of this chronic pain.
Consider your fascial system as an intricate web that may impact your entire body. Myofascial Release can decrease and eventually eliminate soft tissue TMJ tension and jaw joint and/or cartilage misalignment. These may be the real cause of chronic TMD pain.
Constant microtrauma to your jaw’s muscle system can increase oxidative metabolism and quickly deplete cellular energy reserves. This may lead to chronic pain in the myofascial system. It partly derives from the presence of localized area muscular trigger points that become like a taut band. They are tender to palpation and movement, causing local and referred pain.
Palpation during assessment or active movement that generate local pain or referred jaw pain helps to assess the pathophysiology, evaluation, and treatment of myofascial pain and highlights the role of the interprofessional team in managing patients with this condition.
Myofascial pain syndrome is generated by a stimulus, such as jaw muscle tightness, that sets off trigger points that hurt. Meaning, it is also best to have your trigeminal nerve assessed if you have TMJ pain.
Do I need a prescription to manage chronic myofascial pain?
You can first try an over-the-counter painkiller like ibuprofen. If it has gone undiagnosed before reaching the “chronic” stage, you will likely need more relief than ibuprofen provides. Minnesota Head &Pain Clinics seek to start chronic myofascial pain management with conservative treatment strategies. Your pain specialist may prescribe options that are stronger. Many of these medications come in patches you can place on your skin.
SSRIs or antidepressants may relieve chronic myofascial pain, as well. Extreme, persistent pain may be diminished with injections of steroids or a local anesthetic into trigger points.
What are intraoral myofascial therapies?
Intraoral myofascial therapies (IMT) used by physical therapists commonly seek to influence craniofacial structures. Techniques usually involve applying digital pressure (also known as ischaemic compression, pressure release, myotherapy, or acupressure) into masticatory muscle trigger points using intra-oral contact points.
Intra-oral temporalis release is one option. Gloved fingers are placed to apply light pressure on the mandible within the patient’s pain tolerance. Applied superior pressure longitudinally along the temporalis muscle fibers may also be tried. The patient is asked to incrementally open their mouth to its maximum range and work in partnership to assess effectiveness. Commonly, patients prefer other myofascial releases involving the mandibles that are not intraoral.
Does myofascial massage increase blood flow?
Myofascial massage can widen your blood vessels and assist in releasing pain. As the temperature of your fascia increases due to the pressure applied from the hands, it also enables a deeper muscle massage. Myofascial release helps to reduce restriction caused by fascia and also increases blood flow as temperature is increased.
A change in your fascial blood flow (an increase in systolic wave velocity and decreased diastolic velocity due to increased outflow resistance) may trigger myofascial pain. This may further induce an alteration in the morphology and function of the muscular capillaries, leading to reduced blood flow during small active movements. This, in turn, activates type IV nerve endings, contributing to myofascial pain. [1]
According to James Fricton DDS, MS: Professor and Orofacial Pain Specialist, physical therapy or myofascial release can also improve your swallowing function and self-awareness of TMD pain levels and triggers. [3]
Does limited jaw opening indicate a jaw neuromuscular issue?

A low mouth (jaw) opening range is an important indication of the functionality of the temporomandibular joint (TMJ). Mouth opening levels are evaluated by asking the patient to open their mouth as wide as possible and measure the distance between the edges of the frontal incisors and hyoid bone.
Your hyoid bone is located at the root of your tongue in the front of your neck and between your lower jaw and voice box. Assessing its position is part of looking at how to improve jaw functioning. A stimulation of the mesencephalic reticular formation induces rhythmic jaw movements. Myofascial massage may improve your ability to open your jaw with less pain and to function normally.
“As for jaw opening force, hyoid resting position and hyoid dynamics are very important and are considered to be affected directly by the suprahyoid muscles. MFR is found to be effective in giving symptomatic relief and increasing jaw ROM in patients with myofascial TMD. [4]
The C2-through-C5 spinal motion segments are located in the middle portion of your neck (cervical spine). Each segment has 2 adjacent vertebrae and the anatomical structures connecting them. Cervical nerves C1, C2 and C3 (in your neck) control your forward, backward and side head and neck movements. Stresses to the upper cervical spine may cause a reflex to the TMJ muscles, which may cause TMD.
Can someone with jaw pain do self-myofascial release exercises?
While you can simply use your fingers, examples of self‐myofascial release tools are a foam roller and roller massager. Self-myofascial release (SMR) exercise is often used to enhance recovery and performance. You can anticipate best results if managed by an Orofacial Pain Specialist.
How to perform a quick self-evaluation to check for TMJ
- Place a finger over the joint in front of your ear.
- Open your jaw slightly.
- Open wide until you can feel the joint move.
- Listen for clicking or popping when you open your jaw.
- Press gently directly on the joint.
If you feel the joint click or if it’s tender when you press gently, you may have TMJ. You should seek a medical diagnosis if you have prolonged pain or tenderness in your jaw or have restricted jaw movement. Your TMJ specialist can discuss possible causes and provide the best treatment plan based on your symptoms.
There is no widely accepted, standard test available to diagnose TMDs. Because the exact causes and symptoms are not clear, properly identifying these disorders is not possible on your own.
According to the National Institute of Health (NIH), “Self-myofascial release is effective in relieving pain and may improve cycling performance by increasing the iliotibial band flexibility”. [5]
Is myofascial release better than deep tissue massage?
With traditional deep tissue massage, you feel better and gain relaxation with quicker relief from aches and pains than is typically possible on your own. It helps you rejuvenate and keep going. But if you want to address, heal, and get past long-term TMJ aches, pains, and problems, myofascial release therapy is best.
Myofascial Release Techniques Aimed to Improve ROM
Range of motion (ROM) is a common concern for most people suffering from TMJ pain. TMJ massage therapy that addresses the fascial restrictions that form in the tissues due to physical, emotional, or spiritual trauma work in tandem with the established Myofascial Release Protocol. The massage and stretching used in myofascial release therapy can help loosen jaw muscles and joints.
Our clinic has established protocols that take our pain specialists beyond a basic understanding of Temporomandibular Disorder and Craniofacial Pain (CFP). Being experts on the anatomy and biomechanics of TMJ, we offer a comprehensive evaluation and treatment approach.
The following protocol is established by National Institute of Health clinical trials. [6]
NIH Myofascial Release Protocol:
- Suboccipital release.
- Compression – decompression of temporomandibular joint.
- Horizontal release of temporomandibular joint.
- Deep fascia release in temporal region.
- Masseter deep fascia release.
- Pterygoid deep fascia release.
- Intraoral pterygoid deep fascia release.
The myofascial relaxation technique
Myofascial release involves applying gentle pressure into connective tissue and fascia. Facial fascia is a structure of connective tissues that surround muscles, blood vessels and nerves. In healthy conditions, a person’s fascia tissue is relaxed and wavy in configuration.
Fascia plays a vital role in the structure, appearance, and function of your face, jaw, and neck. Your connective tissues benefit from myofascial relaxation. It can be used to prevent TMJ pain from becoming “chronic” or help alleviate it in the chronic stage.
When to see a Pain Specialist for TMJ Pain?
Make an appointment with your doctor or orofacial pain specialist if you experience ongoing jaw muscle pain. Most people occasionally experience muscle pain. But if your head, neck, or jaw muscle pain persists despite rest, massage, and myofascial release self-care measures, make an appointment immediately.
Professional myofascial release treatment can decrease and eventually eliminate soft tissue tension and TMJ-related joint and/or cartilage pain. Treating TMJ with Myofascial Release is achieved using structural releases, gentle jaw joint mobilizations, cranial releases, as well as other customized treatments.
Additionally, many patients with myofascial pain have been found to suffer from a fibromyalgia and TMD relationship. As you can see, diagnosis can be complex; you’ll benefit from professional healthcare.
CONCLUSION: You Can Benefit from Myofascial Release Treatment
Cory Herman, DDS MS, and Patricia Weber, P.T. are members of the University of Minnesota’s TMD, Orofacial Pain and Dental Sleep Medicine Clinic. As we have several Orofacial Pain Specialist that teach there and nationally on the topic.
We will help you get relief from TMD discomfort and pain. Choose our clinic location closest to where you live, call us at:
Plymouth: (763) 577-2484St. Paul: (651) 332-7474Burnsville: (952) 892-6222St. Cloud: 763-233-7252
[1] Cedars-Sinai Health Library, Temporomandibular Disorders (TMD), https://www.cedars-sinai.org/health-library/diseases-and-conditions/t/temporomandibular-disorders-tmd.html, current
[2] Bruno Bordoni, et al, Myofascial Pain, https://www.ncbi.nlm.nih.gov/books/NBK535344/, Aug 2023
[3] James Fricton DDS, Will Suprahyoid Muscle Release be Effective to Improve Myofascial Release Technique, http://science.globalplos.com/149/1/5671-Article%20Text-7804-1-10-20221006.pdf, Indexed by Google in February 2023
[4] Journal of Pharmaceutical Research International, Will Suprahyoid Muscle Release be Effective to Improve Swallowing in Patients with Temporomandibular Disorders?, https://journaljpri.com/index.php/JPRI/article/view/5671, Dec 2021
[5] Jong Jin Park, et al, Effect of Acute Self-Myofascial Release on Pain and Exercise Performance, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9740901/, Dec 2022
[6] NIH, “Miofascial Release and Exercises Therapy in the Treatment of Temporomandibular Disorders”, https://classic.clinicaltrials.gov/ct2/show/NCT02540863, September 2015


