Chronic Pain Providers’ Role in Curbing the Opioid Crisis
Chronic Pain Providers’ Help Curb the Opioid Epidemic
During the pandemic, both the number of people experiencing chronic pain and the opioid epidemic have escalated.
Individuals already suffering from depression or chronic pain who now face additional stress have become more likely to rely on drugs. This is propelling the urgency for chronic pain providers to teach patients how to deal with living in an ongoing painful state without drugs.
The Minnesota Head & Neck Pain Clinic first wrote an article about our concerns in August 2016. It is titled Health Care and Addiction: Instead of Opioids, Prevent Chronic Pain and we remain committed to offering conservative chronic pain treatment.
Table of Contents
- Practices to Reduce Ostensible Risks of Co-Prescribing Opioids
- CDC Addresses Urgency for Less Reliance on Drugs to Treat Pain
- FDA Seeks Non-Addictive Alternatives to Opioids for Acute Pain Management
- US Opioid Use for Chronic Pain and Death Statistics
- Minnesota Opioid Use for Chronic Pain and Death Statistics
- Safe, Effective, Non-addictive Chronic Pain Management Strategies
- Chronic Pain Providers Reporting & Opioid Death Data by State
- Chronic Pain Providers Seek to Reduce Opioid-Related Harms
- Avoiding Opioid Therapy for Sleep Apnea
- SUMMARY: Combating Prescription Opioid Misuse
Practices to Reduce Ostensible Risks of Co-Prescribing Opioids
Pain specialists across the United States are increasingly questioning the ostensible risks of co-prescription of opioids and benzodiazepines. COVID, reports of war, avian flu worries, loneliness, anxiety, and depression are pushing the opioid crisis into focus. It’s now clear that the crisis resides predominantly in the streets and that it will take a united effort to curtail it. Constraining opioid treatment within pain clinics alone is unlikely to suffice.
Thankfully, better medical awareness of this health crisis and new CDC guidelines are both emerging.
CDC Addresses Urgency for Less Reliance on Drugs to Treat Pain
Cautious use of opioids is recommended for the treatment of patients with chronic pain.
A person’s likelihood of developing an opioid use disorder stems from multiple factors. It includes the length of time a person is prescribed to take opioids for acute pain, and how long that individual continues taking opioids (whether as prescribed, or misused). Awareness of the extent of this issue has become a public health crisis and its devastating consequences have increased due to CDC concerns.
The CDC recognizes that patients with pain deserve safe and effective pain management. It states, “Pain, particularly chronic pain, can lead to impaired physical functioning, poor mental health, and reduced quality of life. It contributes to substantial morbidity and mortality in the United States each year. Chronic pain is the leading cause of disability in the United States and the economic costs are staggering—$560 to $635 billion dollars annually.”
It expresses a need for new guidelines that further embrace non-invasive, non-pharmacological and non-opioid pharmaceutical treatment of chronic pain. It recognizes that Opioids have been too often prescribed in response to a jaw tissue injury, or other trauma or surgery. One thing that is clear, the CDC is highlighting of need for chronic pain care providers’ clinical judgment when evaluating drug perscriptions for acute pain care.
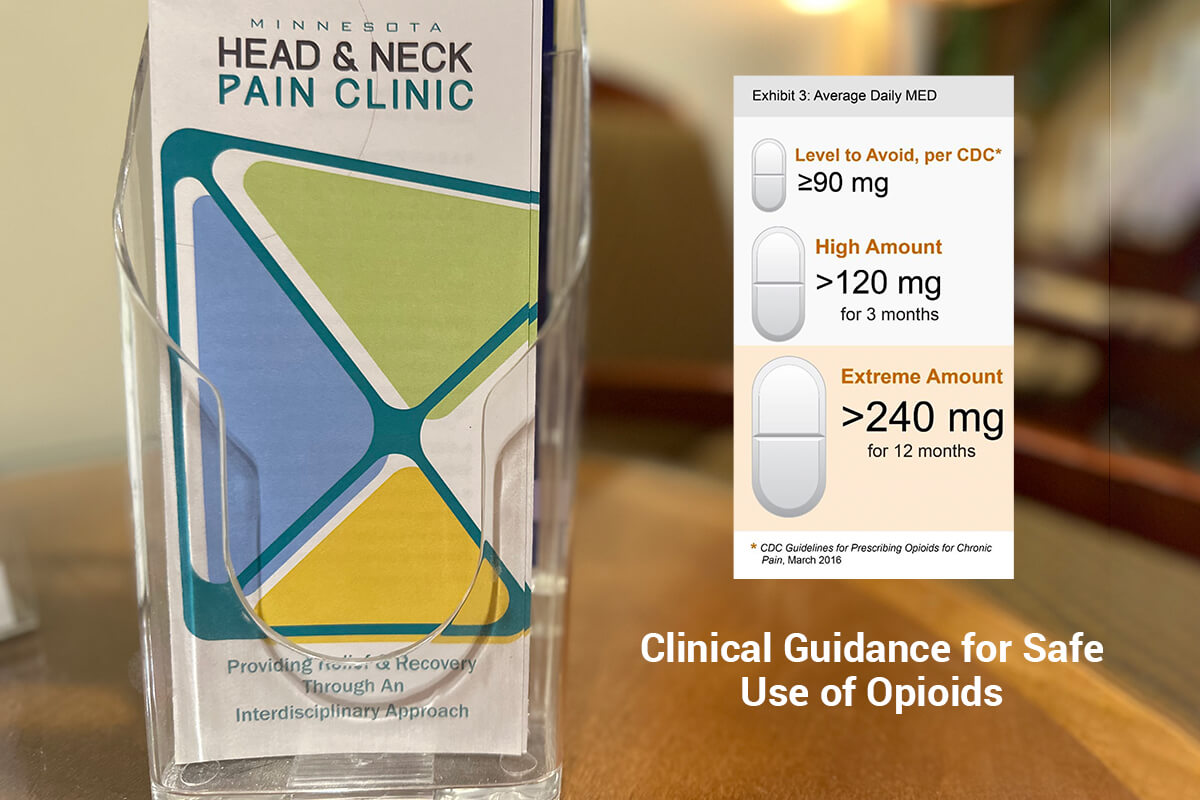
When the CDC wrote new prescribing guidelines in 2016, the intent was to help doctors make better decisions. The document emphasized the risk of opioid addiction, and advised prescribing patients the lowest effective dose. However, our rising crisis puts pressure on chronic pain providers to do more for their patients. Individuals given an opioids prescription need to receive updated and factual information on possible side effects, other risks, and monitoring for safety.
FDA Seeks Non-Addictive Alternatives to Opioids for Acute Pain Management
February 9, 2022, FDA press announcement highlights:
The U.S. Food and Drug Administration took a renewed stance aimed at fostering the development of non-addictive alternatives to opioids to manage acute pain. It also hopes to decrease exposure to opioids and prevent new addictions. The agency issued draft guidance for participants to provide recommendations to companies developing non-opioid analgesics for acute pain lasting up to 30 days.
“Prescribed appropriately, opioid analgesics are an important part of acute pain management. However, even at prescribed doses, they pose a risk for addiction, misuse, abuse, or overdose that may result in death. A non-opioid analgesic for acute pain that completely eliminates or significantly reduces the need for an opioid could have a major public health impact by alleviating patient suffering from acute pain while mitigating the risks associated with using an opioid.”
The Opioid Epidemic is “a public health crisis that has killed half a million Americans and continues to claim tens of thousands of lives every year.” So, how bad is it, really? Let’s look at more statistics.
US Opioid Use for Chronic Pain and Death Statistics
- “Deaths from synthetic opioids are alarmingly high and trending upward. Over the past 12 months, the United States eclipsed 100,000 deaths from illegal drug overdoses for the first time in its history, with more than two-thirds of those deaths caused by illegally produced synthetic opioids.” – David Luckey, MBA, MS
- Roughly 21- 29 percent of patients prescribed opioids for chronic pain misuse them. [1]
- Approximately 25 million US residents have moderate to severe chronic pain, and an estimated 5 million to 8 million of them have used opioids for long-term management, according to National Institutes of Health data.
- Pain is the primary reason Americans are on disability and its societal costs were estimated in 2014 at between $560 and $630 billion annually as a result of missed workdays and medical expenses. [2]
- In 2019, nearly 50,000 people in the United States died from opioid-involved overdoses. [2]
- The United States hit 100,000 overdose deaths in a 12-month period for the first time since such data were recorded. Pain care providers’ strategies and treatment options are predicted to reflect possible FDA policy changes on both a regional and national level. – Bradley D. Stein, MD, PhD, MPH, the director of the Opioid Policies, Tools and Information Center at the RAND Corp., in Pittsburgh.
- Roughly 21 to 29 percent of patients prescribed opioids for chronic pain misuse them. [3].
- Between 8 and 12 percent of people using an opioid for chronic pain develop an opioid use disorder. [3].
- Morbidity, mortality, and financial costs of inadequate treatment of the 18 million Americans with moderate to severe chronic pain are high.
- Overdose deaths involving any opioid increased by 44% from 2,939 in 2019 to 4,233 in 2020 at an average of nearly 12 resident deaths every day during 2020. [4]
- Nationally, overdose deaths were the highest in history with over 91,000 drug-involved overdose deaths and over 68,000 opioid-involved overdose deaths in 2020. [4]
Since our clinics are based in Minnesota, here are some local statistics.
Minnesota Opioid Use for Chronic Pain and Death Statistics
Minnesota, like many other states, is currently experiencing opioid overdose deaths at an epidemic level.
Chronic pain providers have a role in clinical oversite so that drug overdose is more preventable. Below are current MN Department of Health opioid death-related statistics.
- In 2015 Minnesota had over 10,000 treatment admissions for heroin (6485) and other
opiates (3,777). Of these, 34.4% were admitted into OTPs and 65.6% were admitted into abstinence-based treatment programs. - A 2015 analysis of Minnesota state death certificate data found 402 opioid-related deaths in 2016, up from 344.
- In 2019, synthetic opioids were involved in the highest percentage of opioid overdose deaths. The state of MN reported synthetic opioids at 55.38, commonly-prescribed opioids at 25.63%, and Heroin at 19.00%.
- The percentage of Minnesota students using prescription pain medications without a prescription or differently than how a doctor instructed was higher in 2019 than in 2013.
- The amount of methamphetamine seized has increased since 2011, indicating that the supply of methamphetamine has increased in the state of Minnesota.
- In 2020, individuals between 15-34 years of age had the greatest number of ER visits for opioid-involved overdoses. For a breakdown, 1522 cases were reported for residents ages 25-34; and 1126 for residents between the ages of 15 and 24.
- Males had more ER visits than females for opioid-involved overdoses in 2020. 66.12% was attributed to males and 33.88% to females.
- Minnesota prescription-related deaths are second only to alcohol.
- Preliminary reports show 654 opioid-involved deaths in Minnesota in 2020, a 59% increase from 2019
- Approximately 59% of all drug overdose deaths are attributed to opioids, and 18% of those deaths are alcohol-related. Significant increases in the proportion of OOD were found between 2019 and 2020, according to Jessica K. Friedman in Alcohol-related Opioid Overdose Deaths in Minnesota Between 2011 and 2020, published 1.11.2022
“Most common prescription opioid painkillers are Schedule II drugs. This means that any physician may prescribe an opioid painkiller in the course of pain treatment. Opioids are also highly addictive. They activate the brain’s reward systems that trigger the release of dopamine, leading to feelings of intense pleasure.” – Minnesota Opioids, Substance Use, and Addiction Subcabinet and the Governor’s Advisory Council on Opioids, Substance Use, and Addiction; April 7, 2022
A person’s likelihood of developing an opioid use disorder stems from multiple factors. It includes the length of time a person is prescribed to take opioids for acute pain, and how long that individual continues taking opioids (whether as prescribed, or misused).
Awareness of the extent of this issue has become a public health crisis and its devastating consequences have increased due to CDC concerns. It ties into Suicide Awareness concerns when prescribing medications.
Safe, Effective, Non-addictive Chronic Pain Management Strategies
Responding to the opioid crisis, the U.S. Department of Health and Human Services (HHS) is focusing efforts on providing support for cutting-edge research on pain and addiction, as well as advancing better practices for pain management. In Minnesota, our pain clinics focus on reducing overdose by providing easy access to buprenorphine, building interdisciplinary safety plans with our pain patients, and caring for their long-term recovery without any drug dependencies evolving.
Opioid prescription directives have swung over the last five years from the liberal treatment of pain to rigorous restriction to the slow rise in opioid-related deaths when treating chronic pain.
“Opioid misuse and abuse remain a serious public health crisis facing the country. Preventing new addiction through fostering the development of novel non-opioid analgesics is an important priority for the FDA. The guidance reinforces the agency’s commitment to confront opioid misuse, abuse, and addiction by taking steps to help those with acute pain get access to improved non-opioid treatment alternatives.” – Patrizia Cavazzoni, M.D., director of the FDA’s Center for Drug Evaluation and Research.
Chronic Pain Providers and Opioid Death Reporting Data by State
Table 1. Completeness of 12-month ending provisional counts of drug overdose deaths relative to final counts from 2019 after six-month lag, by reporting jurisdiction and ending month
SOURCE: NCHS, National Vital Statistics System, 2019 and CDC Drug Overdose Data. [5]
Coefficients from these updated models were used to update the multiplication factors applied to the reported provisional counts of drug overdose deaths. Model results for each of the ten drug outcomes of interest are presented below. Minnesota has done well in reporting and tracking – data that is helpful to chronic pain providers.
| Reporting jurisdiction | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | oct | Nov | Dec |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| United States | 99.3 | 98.8 | 98.7 | 98.8 | 98.4 | 98.3 | 98.1 | 97.9 | 97.9 | 98.2 | 98.8 | 99.7 |
| Alabama | 95.6 | 96.2 | 98.9 | 96.3 | 95.7 | 99.5 | 98.7 | 96.5 | 97.3 | 98.5 | 99.8 | 99.8 |
| Alaska | 100 | 100 | 86.7 | 100 | 100 | 100 | 100 | 100 | 92.9 | 100 | 100 | 100 |
| Arizona | 98.3 | 99.2 | 99.4 | 100 | 97.1 | 99.3 | 96.5 | 96.9 | 96.8 | 98.7 | 98.9 | 99.7 |
| Arkansas | 100 | 100 | 100 | 100 | 99.5 | 100 | 100 | 100 | 96.7 | 100 | 98.7 | 100 |
| California | 89.2 | 90.4 | 91.9 | 89.5 | 88.5 | 90.9 | 89.2 | 91.7 | 92.2 | 90.3 | 90.9 | 93.7 |
| Colorado | 100 | 98.9 | 97.6 | 99.8 | 100 | 98.8 | 100 | 98.6 | 98.7 | 100 | 100 | 100 |
| Connecticut | 84.3 | 91.3 | 93.1 | 93.5 | 95.6 | 90.4 | 92.1 | 90 | 92.6 | 88.2 | 93.4 | 90 |
| Delaware | 100 | 100 | 93.1 | 100 | 93.7 | 95.7 | 96.7 | 93 | 86.6 | 92.2 | 77.3 | 91.6 |
| District of Columbia | 100 | 100 | 98.9 | 95.7 | 100 | 99.6 | 100 | 97.1 | 98.8 | 99.6 | 100 | 100 |
| Florida | 96.5 | 96.6 | 97.4 | 96.6 | 94 | 94.2 | 93.7 | 95.5 | 95.1 | 94.2 | 97.4 | 98.2 |
| Georgia | 94.9 | 94.4 | 94.1 | 97.2 | 92.1 | 90.3 | 90.5 | 90.6 | 90.4 | 89.6 | 91.5 | 95 |
| Hawaii | 78.2 | 89.9 | 93.6 | 88.9 | 100 | 94.9 | 94.7 | 95.4 | 95 | 100 | 93.9 | 98.2 |
| Idaho | 100 | 100 | 100 | 100 | 100 | 100 | 91.7 | 100 | 95.7 | 95.7 | 100 | 100 |
| Illinois | 95.7 | 99.4 | 98.3 | 97.3 | 97.7 | 99.6 | 98.7 | 98.2 | 98.7 | 96.5 | 96.8 | 97.9 |
| Indiana | 97.1 | 98.3 | 99.1 | 99.1 | 97.2 | 99.3 | 97.9 | 97.1 | 98.9 | 94.2 | 97.2 | 99.9 |
| Iowa | 96.4 | 100 | 100 | 96.7 | 96 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Kansas | 98.8 | 99.7 | 100 | 94.9 | 98.7 | 94.4 | 93.5 | 98.4 | 95.7 | 93.4 | 97.3 | 95.8 |
| Kentucky | 98.8 | 98.5 | 100 | 98.9 | 98.5 | 99.1 | 100 | 97.8 | 99.2 | 99.2 | 100 | 99.8 |
| Louisiana | 99.5 | 98.9 | 100 | 98.7 | 99.6 | 96.7 | 100 | 99.2 | 100 | 98.1 | 99.4 | 99.3 |
| Maine | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 96.2 | 100 |
| Maryland | 98.5 | 100 | 100 | 99.3 | 99.8 | 100 | 100 | 99.9 | 98.9 | 99.5 | 99.3 | 99.3 |
| Massachusetts | 99.8 | 98.6 | 97 | 100 | 100 | 98.9 | 99.1 | 99.5 | 99.5 | 99.1 | 98.4 | 98.7 |
| Michigan | 90.3 | 95.1 | 90.9 | 91.5 | 89.4 | 94.5 | 94.5 | 80.8 | 91.9 | 97.1 | 96.9 | 97.9 |
| Minnesota | 99.8 | 100 | 98.1 | 98.7 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Mississippi | 79.9 | 75.8 | 79 | 94 | 92.2 | 94.2 | 92.9 | 91.1 | 91.9 | 96.7 | 86.3 | 97.8 |
| Missouri | 97.5 | 97.7 | 99.1 | 99 | 97.4 | 97.3 | 100 | 99.9 | 100 | 100 | 99.8 | 100 |
| Montana | 91.3 | 96 | 83.3 | 90.9 | 100 | 66.7 | 85.4 | 96.2 | 90 | 100 | 81.5 | 95.6 |
| Nebraska | 100 | 93.8 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Nevada | 98.4 | 96.7 | 100 | 97 | 100 | 97.2 | 97 | 98.6 | 99.3 | 99.7 | 100 | 99.5 |
| New Hampshire | 6.9 | 21.7 | 50.6 | 76.7 | 97 | 100 | 95.8 | 94.2 | 91.9 | 100 | 97.4 | 100 |
| New Jersey | 90.1 | 93.2 | 92.3 | 91.4 | 94.8 | 94.8 | 91.3 | 97.5 | 96.5 | 97.4 | 97.3 | 98.6 |
| New Mexico | 86.2 | 96.6 | 84.1 | 92.1 | 91 | 90.2 | 97.7 | 96.4 | 95.8 | 95 | 97.1 | 98.8 |
| New York1 | 76.8 | 84.5 | 80.3 | 79.5 | 79.2 | 81.3 | 80.1 | 86.3 | 86.2 | 81.5 | 69.7 | 75.9 |
| New York City | 97.3 | 95 | 95.1 | 98.1 | 95.9 | 99.7 | 100 | 99.4 | 98.9 | 99.2 | 99.9 | 89.2 |
| North Carolina | 74.9 | 74.1 | 72.4 | 74.3 | 71.5 | 72.9 | 79.3 | 66.2 | 59.6 | 54.8 | 63.2 | 75.2 |
| North Dakota | 100 | 100 | 100 | 92.2 | 100 | 100 | 94.4 | 98.2 | 100 | 100 | 100 | 100 |
| Ohio | 97.7 | 97.6 | 94.2 | 95.2 | 93.7 | 95.2 | 95.6 | 95 | 97 | 98.5 | 98.9 | 98.5 |
| Oklahoma | 100 | 97.5 | 95.9 | 100 | 95.2 | 100 | 94.8 | 94.1 | 99.4 | 100 | 100 | 98.5 |
| Oregon | 94.6 | 97.7 | 91.8 | 90.1 | 95.1 | 94.6 | 91.9 | 93.1 | 93.4 | 90.9 | 94.1 | 87.2 |
| Pennsylvania | 95.8 | 94.3 | 95.3 | 92.9 | 95.5 | 97.1 | 95.2 | 94.3 | 94.1 | 93.3 | 95.3 | 97.3 |
| Rhode Island | 100 | 97 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| South Carolina | 90.5 | 97.3 | 95.1 | 92.2 | 88.7 | 97.9 | 93.2 | 94 | 97 | 90.7 | 90.1 | 96.6 |
| South Dakota | 75 | 100 | 100 | 100 | 100 | 98.9 | 100 | 100 | 100 | 100 | 100 | 100 |
| Tennessee | 84.6 | 83.5 | 90.4 | 88.3 | 90 | 93.1 | 97.1 | 96.2 | 95.5 | 95.4 | 96.6 | 98.2 |
| Texas | 68.5 | 75.8 | 86.6 | 96.8 | 92.7 | 95.3 | 95.1 | 97 | 96.2 | 96.3 | 96.8 | 98.5 |
| Utah | 88.7 | 97.9 | 100 | 100 | 96.1 | 96 | 100 | 100 | 100 | 100 | 99.8 | 100 |
| Vermont | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Virginia | 99.2 | 98.4 | 99.2 | 09 | 97.7 | 95.6 | 96.7 | 94.8 | 99.8 | 99.4 | 98.8 | 100 |
| Washington | 93.3 | 92.6 | 89.5 | 94.9 | 96.4 | 90.2 | 91.9 | 91.2 | 86.8 | 79.1 | 75.3 | 77 |
| Wisconsin | 92.4 | 94.4 | 96.4 | 97.5 | 94.2 | 95.9 | 93.9 | 99.4 | 95.2 | 96.9 | 99 | 98.4 |
| Wyoming | 100 | 100 | 100 | 100 | 66.7 | 100 | 100 | 98 | 100 | 100 | 100 | 100 |
| Wisconsin | 92.4 | 94.4 | 96.4 | 97.5 | 94.2 | 95.9 | 93.9 | 99.4 | 95.2 | 96.9 | 99 | 98.4 |
| Wyoming | 100 | 100 | 100 | 100 | 66.7 | 100 | 100 | 98 | 100 | 100 | 100 | 100 |
Chronic Pain Providers Seek to Reduce Opioid-Related Harms
Many pain patients need professional support through a very difficult time and thought leaders who give attention to their long-term reduced pain plan. According to the Drug Enforcement Administration, opioid-related deaths are being fueled partly by illicit fentanyl. Even a minuscule amount, the size of one small grain of salt of illicit fentanyl can be fatal to an adult.
Chronic pain treatment with the intent to improve the success rate of opioid tapering is important to the state of Minnesota and the MN Head and Neck Pain Clinics. Answers to pain patients’ questions are important to empower them when formulating effective interventions and treatment plans. Slower pain perscription tapers (like, 10% per month or slower) are often better tolerated than more rapid tapers, especially following opioid use for more than a year.
Acute pain patients can benefit from educational sources that focuses on:
- Opioid alternatives for pain management.
- How to identify and address co-existing mental health conditions (e.g., depression, anxiety, PTSD).
- Early diagnosis of neuropathic pain from TMD.
- How to manage opioid reversal.
- Why a lower duration of and proper opioid use is critical.
- Setting pain management expectations with reduced prescription use.
- How to dispose of un-needed opioids when pain levels subside.
- How to increase peer and family support during acute pain treatment.
- How mindfulness-based pain treatment therapy can decrease opioid dependency.
These patients are best served by chronic pain providers’ multidisciplinary approach to their care. It often includes behavioral medicine, psychologists, and is assisted by physical therapists. Chronic pain providers focus on patient safely, satisfaction, better emotional function and lower pain level outcomes.
Quality, compassionate, multidisciplinary care reduces opioid misuse
Limiting opioid prescription use is one effort to help but may limit access for vulnerable people to the healthcare resources they seek. These people struggling with anxiety, depression, or emotional issues should not feel left alone or in a state that prompts them to addiction drawing from illicit sources. They need access to chronic pain management that can safely meet their needs.
Our chronic pain experts advocate for clinician–patient engagement that allows for sufficient time to establish a reasonable rapport of trust. This requires an infrastructure to be in place that permits pain specialists to do that. It requires adequate time (and reasonable compensation) to provide quality, compassionate, multidisciplinary care and the visit frequency that can make a difference in this opioid crisis.
To effectively wean chronic pain patients from opioids, clinicians need flexibility in opioid prescribing best practices. It’s good to see increased awareness and commitment to retaining pain patient engagement, providing better self-care boundaries, and minimizing prescription risks.
As the CDC and other groups take a hard look at policy that regulates opioid prescriptions to pain patients. Hopefully, it will lower the current rising rates of death by suicide and opioids.
People with ongoing acute pain commonly face additional health issues.
CDC recommendations: preventative non-opioid pain treatments for migraine headaches:
- Beta-blockers
- TCAs
- Antiseizure medications
- Calcium channel blockers
- Nonpharmacological treatments (Cognitive behavioral therapy, relaxation, biofeedback, exercise therapy)
- Avoid migraine triggers
The above less-addictive headache treatment options have been shown to work well in helping limit the number of migraines you get. The best help is to diagnose the cause and eliminate it or reduce its impact. They do have side effects, though, when prescribed in high doses for tension headache types, too.
Avoiding Opioid Therapy for Sleep Apnea
A strong correlation exists between chronic pain patients and sleep disturbances.
Opioids may affect a person’s control of breathing and impair upper airway function. A pain patient using prescription opioid treatment may find it causing central apneas, upper airway obstruction, and hypoxemia during sleep. Care is easier today than ever. COVID prompted a rise in telehealth chronic pain care treatment without needing to come into a clinical office.
Past research surfaces concerns for a correlation between chronic opioid therapy (COT) and sleep-disordered breathing (SDB) and the increased risk for unintentional opioid-related overdose when treating central sleep apnoea (CSA). Oral appliance use is a much safer way to treat lack of sleep issues.
Further research is needed to better determine the effect of prescription opioids on sleep quality and pain intensity and the risks associated with opioids and SDB. The continuing rise of acute pain patients with prescription opioid dependence is a strong stimulus for future research.
“Patients with chronic pain who report significant sleep disturbance endorse higher rates of depression and anxiety as well as greater pain intensities. Studies have demonstrated a bidirectional relationship between pain and sleep; poorly controlled chronic pain can reduce sleep quality and conversely poor sleep quality can increase pain intensity.” – Opioid Therapy and Sleep Disorders: Risks and Mitigation Strategies [6]
Dr. Cory Herman’s Effective Oral Appliances for Treating Sleep Apnea January 6, 2022 article covers help for sleep disorders without the use of opioid therapy. Recognize that we all play a role in tackling the deathly grip these drugs currently hold on many of our loved ones and Minnesota communities.
SUMMARY: Combating Prescription Opioid Misuse
The MN Head & Neck Pain Clinic is a leader in providing safe and conservative care for Americans who have relied on opioid treatment to manage chronic pain. We must remind ourselves that pioid use — even short term — often leads to addiction and overdose. The odds you or someone you love will still be on opioids a year after taking a short perscription increase after only five days on opioids. We care that our patients can contribute to society and enjoy a higher quality of life than addiction.
To recap, prescription opioids used for pain relief are generally safe when taken for a short time and as prescribed by a pain specialist, but they can be so easily misused. Patients are protected from long term opioid prescription drug use, in most cases, by starting out with safer pain treatment options and better clinical judgement.
People with questions or requests for additional information may contact info@mhnpc.com.
Supplemental Readings:
CDC Guidelines for Prescribing Opioids 2016
Guidelines for Prescribing Opioids for Chronic Pain
CDC Non-addictive Strategies to Manage Chronic Pain
Minnesota Opioids Substance Use and Addiction Subcabinet
Minnesota State Targeted Response to the Opioid Crisis, April 2017
References:
[1.] National Institute on Drug Abuse: Opioid Overdose Crisis; https://nida.nih.gov/drug-topics/opioids/opioid-overdose-crisis
[2.] NIH Pathways to Prevention Workshop: The Role of Opioids in the Treatment of Chronic Pain; https://prevention.nih.gov/sites/default/files/documents/programs/p2p/ODPPainPanelStatementFinal_10-02-14.pdf
[3.] CDC/NCHS, National Vital Statistics System, Mortality. CDC WONDER, Atlanta, GA: US Department of Health and Human Services, CDC; 2019. https://wonder.cdc.gov.
[4.] Vowles KE, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain. 2015; 156(4):569-576. doi:10.1097/01.j.pain.0000460357.01998.f1. https://nida.nih.gov/drug-topics/opioids/opioid-overdose-crisis
[5.] https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
[6.] https://watermark.silverchair.com/16-suppl_1-S22.pdf
Article research and statistical data by Hill Web Marketing, management of healthcare content strategies.



